Mental Health Challenges and Interventions in Veterans with Combat Experience
Mental Health Challenges and Interventions in Veterans with Combat Experience
Veterans who have experienced combat face a unique set of mental health challenges. The impact of their service extends far beyond the battlefield, affecting their psychological well-being, relationships, and daily functioning. In this article, we delve into the mental health issues commonly faced by these brave individuals and explore evidence-based interventions that can aid in their recovery and improve their quality of life.

Combat experience often exposes veterans to traumatic events, which can lead to a range of psychological issues. The most prevalent among these is Post-Traumatic Stress Disorder (PTSD), characterized by symptoms such as flashbacks, hyperarousal, and avoidance behaviors. However, PTSD is not the only concern; veterans may also experience depression, anxiety, substance abuse, and difficulties with anger management.
Prevalence of PTSD in Veterans
Studies have shown that the prevalence of PTSD among veterans varies, depending on the conflict and individual experiences. For instance, a report by the U.S. Department of Veterans Affairs estimates that about 11–20% of veterans who served in Operations Iraqi Freedom (OIF) and Enduring Freedom (OEF) suffer from PTSD in a given year (Department of Veterans Affairs, 2021).
Co-occurring Disorders
Many veterans with PTSD also struggle with co-occurring disorders such as depression and substance abuse. A study by Seal et al. (2011) found that nearly one-third of veterans seeking treatment for PTSD also had a substance use disorder, and more than half were diagnosed with depression.
Evidence-Based Interventions for Veterans
Effective treatment for veterans with combat-related mental health issues involves a combination of psychotherapy, medication, and holistic approaches. Tailoring these interventions to the individual’s needs is crucial for successful outcomes.
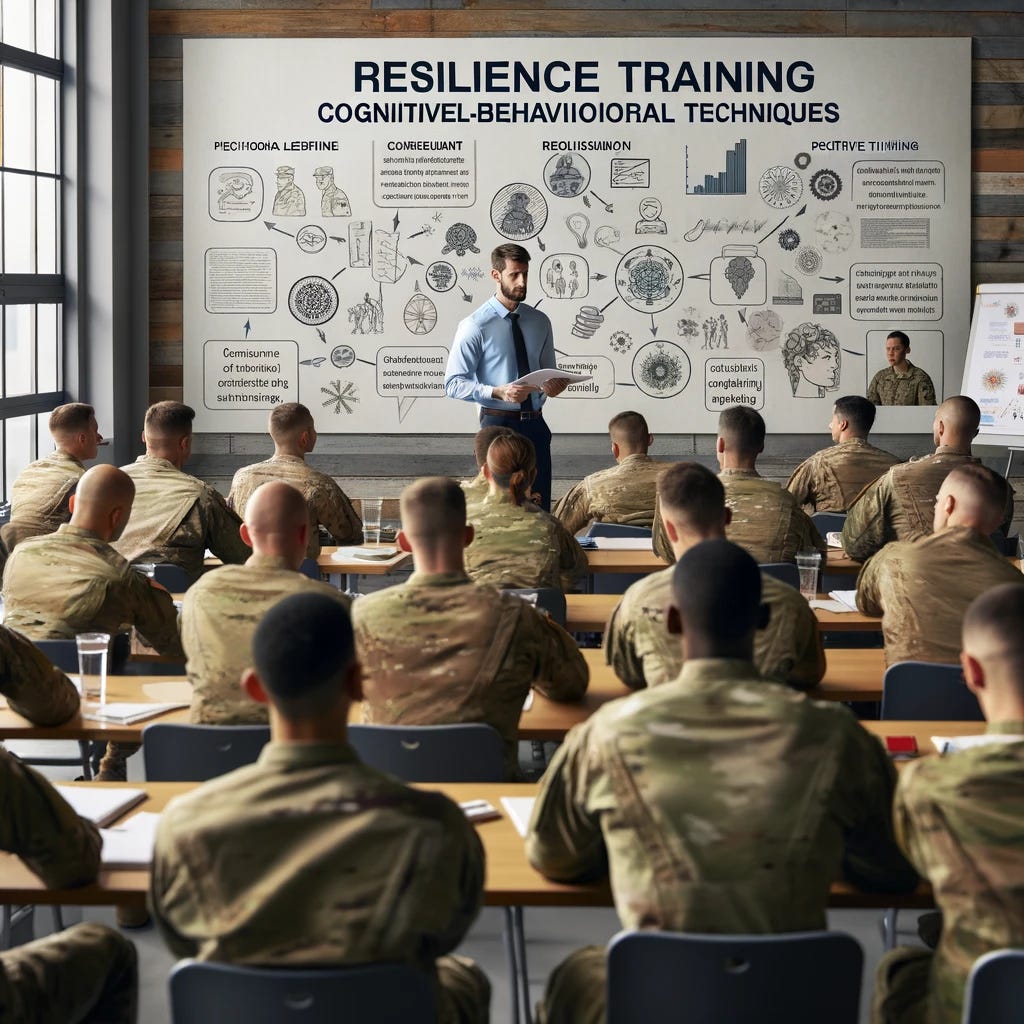
Cognitive-Behavioral Therapy (CBT)
CBT is a widely used psychotherapeutic approach that helps individuals recognize and alter dysfunctional thoughts and behaviors. It has been particularly effective in treating PTSD and associated conditions in veterans. Prolonged Exposure Therapy (PET) and Cognitive Processing Therapy (CPT), both forms of CBT, have shown significant success in reducing PTSD symptoms (Resick et al., 2017).
Eye Movement Desensitization and Reprocessing (EMDR)
EMDR is another therapy that has garnered attention for its effectiveness in treating PTSD. This therapy involves recalling traumatic memories while simultaneously focusing on external stimuli, usually guided eye movements, which helps reduce the intensity of distressing memories (Shapiro, 2018).

Medication Management
Medications, particularly selective serotonin reuptake inhibitors (SSRIs), are often prescribed to veterans with PTSD to alleviate symptoms of depression and anxiety. Research indicates that SSRIs, in combination with psychotherapy, can significantly improve outcomes for veterans with PTSD (Bernardy & Friedman, 2015).
Holistic and Alternative Therapies
Incorporating holistic and alternative therapies such as mindfulness, yoga, and acupuncture can enhance the effectiveness of traditional treatments. These approaches focus on the mind-body connection, helping veterans manage stress and improve overall well-being (Libby et al., 2012).
Addressing Unique Challenges Faced by Veterans
Veterans with combat experience may face unique barriers to seeking and receiving mental health treatment. Stigma, lack of understanding from non-military mental health providers, and logistical challenges like access to care are significant hurdles.
Overcoming Stigma
Stigma surrounding mental health issues can prevent veterans from seeking help. Efforts to normalize mental health treatment and educate both veterans and the public about the realities of mental health challenges can help reduce this barrier (Acosta et al., 2014).
Culturally Competent Care
Providing culturally competent care, which acknowledges and respects the unique experiences and values of veterans, is essential for effective treatment. Mental health professionals need to understand military culture and the specific stressors associated with combat experience (Tanielian & Jaycox, 2008).
Access to Care
Improving access to care, especially in rural and underserved areas, is crucial. Telehealth services have emerged as a promising solution, offering veterans remote access to mental health care regardless of their location (Tuerk et al., 2010).

FAQs
Q1: What are the common mental health issues faced by veterans with combat experience? Common issues include PTSD, depression, anxiety, substance abuse, and difficulties with anger management.
Q2: How effective is Cognitive-Behavioral Therapy (CBT) in treating PTSD in veterans? CBT, particularly Prolonged Exposure Therapy and Cognitive Processing Therapy, has been shown to be highly effective in reducing PTSD symptoms.
Q3: Can medications help veterans with PTSD? Yes, medications, particularly SSRIs, can alleviate symptoms of depression and anxiety when combined with psychotherapy.
Q4: What are the barriers to mental health treatment for veterans? Barriers include stigma, lack of culturally competent care, and limited access to mental health services.
Q5: Are alternative therapies beneficial for veterans with mental health issues? Yes, holistic and alternative therapies like mindfulness, yoga, and acupuncture can complement traditional treatments and enhance overall well-being.
For More Information:
- Department of Veterans Affairs: www.va.gov
- National Center for PTSD: www.ptsd.va.gov
- Mental Health America: www.mhanational.org
- American Psychological Association: www.apa.org
References
- Acosta, J. D., Becker, A., Cerully, J. L., Fisher, M. P., Martin, L. T., Vardavas, R., … & Schell, T. L. (2014). Mental Health Stigma in the Military. RAND Corporation.
- Bernardy, N. C., & Friedman, M. J. (2015). Pharmacological management of posttraumatic stress disorder. Current Opinion in Psychology, 1, 6–11.
- Department of Veterans Affairs. (2021). PTSD: National Center for PTSD.
- Libby, D. J., Pilver, C. E., & Desai, R. (2012). Complementary and alternative medicine in VA specialized PTSD treatment programs. Psychiatric Services, 63(11), 1134–1136.
- Resick, P. A., Monson, C. M., & Chard, K. M. (2017). Cognitive processing therapy for PTSD: A comprehensive manual. Guilford Publications.
- Seal, K. H., Cohen, G., Waldrop, A., Cohen, B. E., Maguen, S., & Ren, L. (2011). Substance use disorders in Iraq and Afghanistan veterans in VA healthcare, 2001–2010: Implications for screening, diagnosis and treatment. Drug and Alcohol Dependence, 116(1–3), 93–101.
- Shapiro, F. (2018). Eye movement desensitization and reprocessing (EMDR) therapy: Basic principles, protocols, and procedures. Guilford Publications.
- Tanielian, T., & Jaycox, L. H. (Eds.). (2008). Invisible wounds of war: Psychological and cognitive injuries, their consequences, and services to assist recovery. Rand Corporation.
- Tuerk, P. W., Yoder, M., Ruggiero, K. J., Gros, D. F., & Acierno, R. (2010). A pilot study of prolonged exposure therapy for posttraumatic stress disorder delivered via telehealth technology. Journal of Traumatic Stress, 23(1), 116–123.
Dr. Jerry D. Smith Jr. is a clinical psychologist and empathic expert specializing in human empowerment and leadership.
More from Dr. Jerry Don Smith Jr. and Operational & Defense Psychology Review